For approximately 1/3 of couples that have a fertility problem, the complication stems from male factor infertility.
A vasectomy reversal, or vasovasostomy, is a surgical procedure to reconnect the tubes that are cut during a vasectomy (Figure 1). These tubes (called the vas deferens) are each about the size of a strand of spaghetti, and the channels in the tubes that conduct sperm are barely visible to the naked eye. Sperm production continues after a vasectomy, but with no place to go the sperm are reabsorbed.
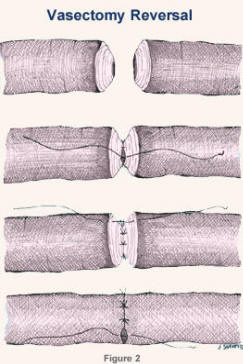
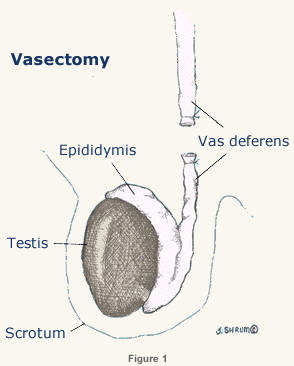
During the reversal, the vas deferens is cut above and below the site of the previous vasectomy, and the two ends are precisely aligned. Dr. Generao uses an operative microscope and performs a “three-layer” connection (Figure 2). Less precise procedures are performed by some doctors because they take less time and do not require as much surgical skill.
In the United States, physicians are currently performing about 500,000 vasectomies per year. About 1 percent of men (1 out of 100) who have had a vasectomy will decide to undergo a reversal. The technique used for the vasectomy is largely irrelevant to the success of the reversal. The vas deferens is a long tube and it is very rare to be unable to accomplish a reconnection.
After vasectomy reversal:
| Years Since the Vasectomy | Sperm in the Ejaculate |
|---|---|
| <5 | 97 % |
| 5-10 | 90-95 % |
| 10-15 | 85-90 % |
| >15 | 80-85 % |
Pregnancy rates are never as high as the “surgical success” rates shown in this table. The pregnancy rates that result from intercourse at home will generally be lower, and are significantly dependent on the age of the woman. For most couples who opt for the reversal within five years of the vasectomy, “home” pregnancy rates range from 65 to 75 percent; reversals done 10 to 20 years from the vasectomy result in pregnancies in 55 to 65 percent of cases. However, pregnancy rates can be made even higher if a couple is willing and able to pursue assisted reproductive techniques, such as intrauterine insemination or in vitro fertilization.
There are three main reasons for this:
There are two important points to make about the “success” table:
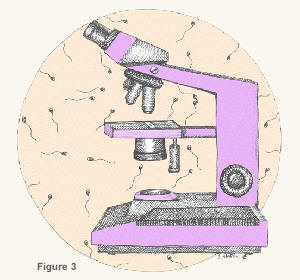 Let’s discuss this last point in more detail. We know that certain findings at the time of the vasectomy reversal will give us more information about the chances of success. When the reversal is done, the vas deferens is cut between the testis and the vasectomy site. The fluid that comes out of the vas deferens can be examined with a microscope in the operating room (Figure 3).
Let’s discuss this last point in more detail. We know that certain findings at the time of the vasectomy reversal will give us more information about the chances of success. When the reversal is done, the vas deferens is cut between the testis and the vasectomy site. The fluid that comes out of the vas deferens can be examined with a microscope in the operating room (Figure 3).
Thick fluid without sperm is almost always a sign that the delicate tubes on the side of the testis (called the epididymis) have become blocked. It is possible to bypass the epididymal block by performing a vasoepididymostomy (don’t try to pronounce this word!).
A vasoepididymostomy is a surgical procedure in which the vas deferens is hooked up directly to the epididymis above the blockage (Figure 4). Generally, the success rate of vasoepididymostomy (as defined by sperm in the ejaculate after surgery) is about 75-80 percent. This is very significant compared with the 10 percent rate of success following a standard vasectomy reversal when the fluid is thick and devoid of sperm.
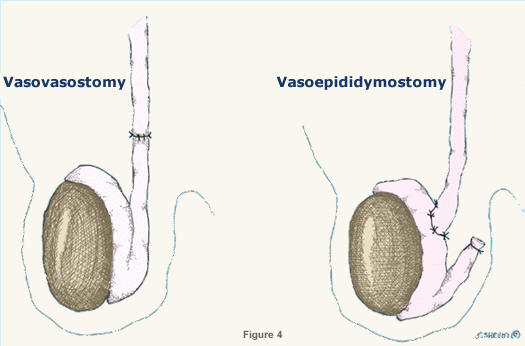
So keep in mind that the success rates in the table above will be higher if the surgeon is prepared to perform a vasoepididymostomy if an epididymal block (thick fluid) is suspected at surgery. We will attempt to identify cases with epididymal obstruction. (See next question).
One final point: The fluid findings at surgery may be equivocal for epididymal blockage. For example, the fluid may be thick but nonetheless contain sperm or sperm fragments. Alternatively, the fluid may be thin or scant but may not contain sperm or sperm fragments. In these cases, it is not clear if the epididymis is blocked or not. Your doctor will weigh all of the relevant factors and perform the type of connection with the highest chance of success. In some cases, it may be necessary to perform the delicate vasoepididymostomy on one side and the “standard” vasectomy reversal on the other.
On the average, one vasoepididymostomy for every 10 to 15 standard vasectomy reversals (vasovasostomies). However, the longer it has been since your vasectomy, the more likely it is you will need this procedure.
It is very rare to find large numbers of active sperm at the cut end of the vas deferens during a reversal. It would be possible to expose the epididymis, “nick” a tubule and recover active sperm, but this increases the risk of obstructing the epididymis at the site of the “nick”. For this reason, we generally do not recommend freezing sperm during a vasovasostomy.
However, if a vasoepididymostomy is required, freezing sperm becomes quite feasible. During the course of a vasoepididymostomy, the epididymis tubule is “nicked” to check for active sperm. In this setting, it is very reasonable to collect and freeze epididymal sperm.
Two important points should be clearly understood:
In vitro fertilization (IVF), with micro-injection of sperm, (Intracytoplasmic Sperm Injection – ICSI) would be necessary to assist the fertilization process.
A small opening will be made on each side of your scrotum to gain access to the vas deferens and the re-connection will be performed.
Typically, the surgery takes about three hours for a standard reversal and about four hours if you need a vasoepididymostomy. The sedative will probably make you sleep for most of the procedure. When your surgery is finished, you will spend a short time in the recovery room before you are sent home. You will be given printed postoperative instructions regarding activity restrictions and follow-up.
It is very rare to have a serious complication from a vasectomy reversal. The most common complications are:
There is no reason why this type of surgery should affect either urination or erections.
Contrary to popular belief, most men are not in severe pain after surgery. Some men tell us that the vasectomy was much worse! Ice is applied to the scrotum for about 36 hours following surgery and a pain pill may be used as needed. Warm soaks are started after 72 hours. Walking and light activity are resumed quickly but heavy lifting and vigorous exercise are restricted for four weeks. Sexual intercourse is avoided for ten days. Most men are able to return to work after only a few days.
Sperm are commonly seen at one month if a standard reversal was performed. If a vasoepididymostomy was performed, it may take several months before sperm are seen.
We’ve had patients conceive within two weeks of surgery! However, data collected on large numbers of vasovasostomy patients show a mean (average) time between surgery and pregnancy of about 6 to 12 months, depending on female age and time since vasectomy.
Since pregnancies do not usually occur right away, most couples will not want to delay surgery. If you do not plan to conceive for several years, then a delay might be reasonable.
There are data that show a deterioration of semen quality over time in 5 to10 percent of men after vasovasostomy and in 10 to 20 percent of men after vasoepididymostomy. Sperm banking may be considered but this does not guarantee success.
Problems such as these appear to occur at the same frequency as in the general population.
It is now possible to extract sperm cells from the testicle or epididymis. However, we do not recover enough sperm to produce a pregnancy by simply inseminating the woman. Instead, the sperm are used in the laboratory to fertilize eggs removed from the female partner (in vitro fertilization – see question 16). These lab techniques are much more costly than the reversal itself but they do represent a viable option with good success rates for couples who can afford them. Therefore, in most cases, a vasectomy reversal is more cost effective and the best first option.
If you had a previous vasectomy reversal and now have no sperm, a “re-do” reversal may be a reasonable option. Success rates for re-do reversals are still very good, declining by only about 5 percent compared with the “first try”. If sperm were ever seen after the first attempt, this is a good sign that a re-do could restore sperm to the ejaculate.
There are several techniques that can help to produce a pregnancy if it doesn’t occur at home. Intrauterine insemination (IUI) of sperm can be performed in some situations (if the sperm count is adequate). With this procedure, the woman’s cycle is monitored to detect the time of ovulation. At the appropriate time, a sperm sample is collected, washed, and concentrated. The sample is then placed into the upper uterine cavity by means of a small catheter.
Depending on the quality and quantity of sperm, some couples will require in vitro fertilization (IVF) in order to conceive. IVF is a technique where eggs are removed from the woman’s ovaries and placed in a lab dish with sperm. Success rates depend upon the age of the woman and the quality of the resulting embryos.
If the sperm count is very low, an assisted fertilization procedure may be necessary. This procedure, known as intracytoplasmic sperm injection (ICSI) is utilized in an IVF cycle and consists of injecting a single sperm into each egg. For those men who do not have any sperm in the ejaculate after vasovasostomy or those who elect not to have a reversal, sperm may be obtained surgically by percutaneous sperm extraction (with needle) or open sperm extraction (with minor surgery).
Adoption or insemination with donor sperm are also other options for couples who are unable to conceive following a vasectomy reversal.
Making the decision to reverse a vasectomy is a big step. Considering all of the options currently available, vasectomy reversal represents the most cost effective option for having your own biological child in most cases. We will make every effort to make your experience as comfortable and convenient as possible. Please ask questions! We look forward to meeting you!
We are currently able to offer one global fee for vasovasostomy (vasectomy reversal) and if necessary, vasoepididymostomy (correction of epididymal obstruction). The total fee is $7,700.00. This global fee covers all aspects of the reversal including the “pre-op”, surgery fees (professional and facility fees), and two postoperative semen checks. The global fee does not cover the sperm freezing option as discussed earlier.
Most of our patients find that their insurance company will not pay for the reversal. You may wish to submit a claim to your insurance company and we would be happy to assist you in doing so.
We are extremely proud that this global fee is much lower than comparable fees around the United States. Other programs offer this same arrangement for as much as $25,000.00. Remember that this global fee will cover not only a bilateral vasectomy reversal but will also cover the more delicate correction of epididymal blockage if it is found.
Please call our office if you have any questions about the microscopic vasectomy reversal program.
You may want to have your semen checked after surgery. This can be done anytime; most people wait about 4-8 weeks after surgery if a standard vasectomy reversal was done on either one or both sides. If a vasoepididymostomy was done on both sides, it is preferable to wait 8-12 weeks after surgery before the semen is checked. Abstain from ejaculation for about 2-3 days prior to any type of post-operative semen testing. To schedule a post-operative semen check please call our office.
For the most current list of fees, please visit Vasectomy Reversal Costs