What is endometriosis?
Endometriosis occurs when the lining of the uterus (endometrium) implants in the pelvis outside of the uterus. The endometrium is shed each month during the menstrual period and exits the uterus not only via the cervix and vagina, but also via the fallopian tubes into the pelvis. If the tissue implants onto the pelvic organs it can be associated with chronic inflammation, growth of new blood vessels (angiogenesis), and increased nerve density within the pelvis. This may cause pain, including severe pain with periods (dysmenorrhea), pain with intercourse (dyspareunia) and pain with bowel movements (dyschesia). Irritable bowel syndrome symptoms occurring at the time of a period may also be associated with endometriosis.
Implants on the ovaries may result in ovarian cysts called endometriomas, which can also be painful.
How common is it?
Endometriosis affects approximately 10% of reproductive aged women and can occur at any time from the onset of menstrual periods to menopause. It most commonly causes symptoms in women in their 30’s and 40’s.
It is found in 50% of women who are infertile and in 60% of women with chronic pelvic pain.
It is classified in four stages from minimal, mild, moderate to severe and symptoms do not always reflect the severity of the disease. Some women have no symptoms and only find out they have endometriosis after having a laparoscopy performed in the course of a workup for infertility.
What factors affect the possible development of endometriosis?
There is a genetic component, with 9% of women with the disease having affected first degree relatives. Research is showing that there appear to be several hundred gene mutations that are correlated with surgically confirmed disease. However, chemical modification of inherited DNA (epigenetic changes) are likely very important in determining who develops the disease and who does not. Environmental toxins such as endocrine disrupting compounds (e.g. phthalates) have been implicated in increasing the chance of developing endometriosis. Diet may also modify the risk: diets high fruit, vegetables, and healthy fats may decrease the risk.
How is endometriosis diagnosed and treated?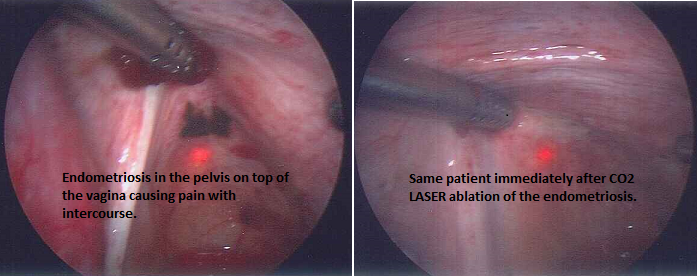
Since pain is often associated with normal menstrual periods, it may take years to make the diagnosis in any given woman. If severe pain with periods is not relieved by NSAIDS (e.g. ibuprofen, naproxen sodium) endometriosis should be suspected. If a woman is not actively trying to conceive, added treatment with other medications including continuous contraceptives (birth control pills, patch or vaginal ring) or a course of a GnRH (gonadotropin releasing hormone) agonist such as leuprolide acetate or nafarelin acetate may be tried to see if pain relief can be achieved. These medications stop menstrual periods and in the case of the GnRH agonists, decrease estrogen levels. If pain is significantly relieved, the contraceptive or the GnRH agonist (with add-back progestin to prevent hot flushes and loss of bone density) can be continued. New medications, such as oral forms of GnRh antagonists are under development. These lower estrogen production by the ovaries like GnRH agonists, but work more quickly and appear to be less likely to cause hot flushes or to decrease bone density.
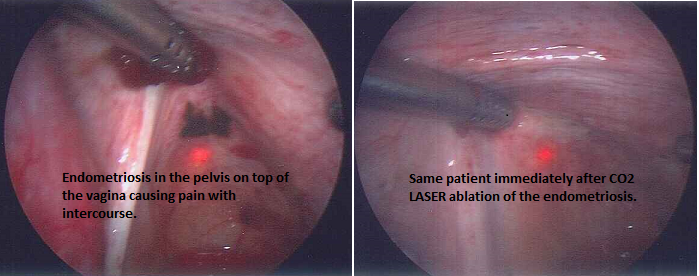
If pain is not relieved with these medications or a woman is desirous of conception, then surgery by laparoscopy is recommended. This allows visual diagnosis of the disease as well as treatment by ablation or excision of implants and removal of scar tissue (e.g. with lasers) and excision of ovarian cysts. Surgical treatment can relieve pain and can improve chances for conception.
In addition to this, pelvic ultrasound can make a presumptive diagnosis of endometriosis by identifying endometriomas (ovarian cysts which have a very characteristic appearance on ultrasound). These cysts cannot be successfully treated with medication and if they are causing pain or are 4 to 5 cm or larger in diameter, surgery is generally recommended to excise them.
To date, there is no blood test for diagnosis of endometriosis; however, active research for biomarkers is ongoing. One promising area is that of microRNA’s in serum which may have future potential as markers for this disease.
Treatment
If mild to moderate endometriosis is diagnosed and treated at time of laparoscopy, it is usually recommended that the woman be treated with fertility medications postoperatively to maximize chance for pregnancy, as the chance that the disease will recur is approximately 40%. Recurrence may take many months or may occur quickly.
If severe disease is found at the time of surgery, with the presence of extensive implants, tubal distortion, and severe scarring in the pelvis, in vitro fertilization is often recommended in order to optimize chances for pregnancy.
The reproductive endocrinologist treating the woman will discuss all options and make individualized recommendations based on that particular patient’s situation.
Have you been dealing with chronic endometriosis and are having a difficult time conceiving? Contact us here at Northern California Fertility Medical Center, Sacramento’s premier fertility and IVF center for nearly 30 years.
References:
Reproductivefacts.org: Endometriosis: A Guide for Patients (Booklet)
Endometriosisjourney.com
Muzii, Ludovico et al. Management of Endometriomas. Seminars in Reproductive Medicine. 2017; 35(1): 25-30.
Bedaiwy, Mohamed et al. New developments in the medical treatment of endometriosis. Fertility and Sterility. March 2017; 107(3): 555-565.